Renal perfusion status is monitored closely in a client who has had abdominal aneurysm repair. Hypotension, dehydration, prolonged aortic clamping during surgery, blood loss, or embolization can lead to decreased renal perfusion and potential kidney injury. The nurse should routinely monitor the client's blood urea nitrogen (BUN) and creatinine levels as well as urine output. Urine output should be at least 30 mL/hr. This client should have an output of at least 120 mL of urine in a 4-hour period.
(Option 1) Diminished breath sounds in the lung bases are a common occurrence after surgery, especially in a client who has an abdominal incision that is painful with deep inspiration. The nurse should medicate the client for pain and encourage coughing, deep breathing, and use of an incentive spirometer.
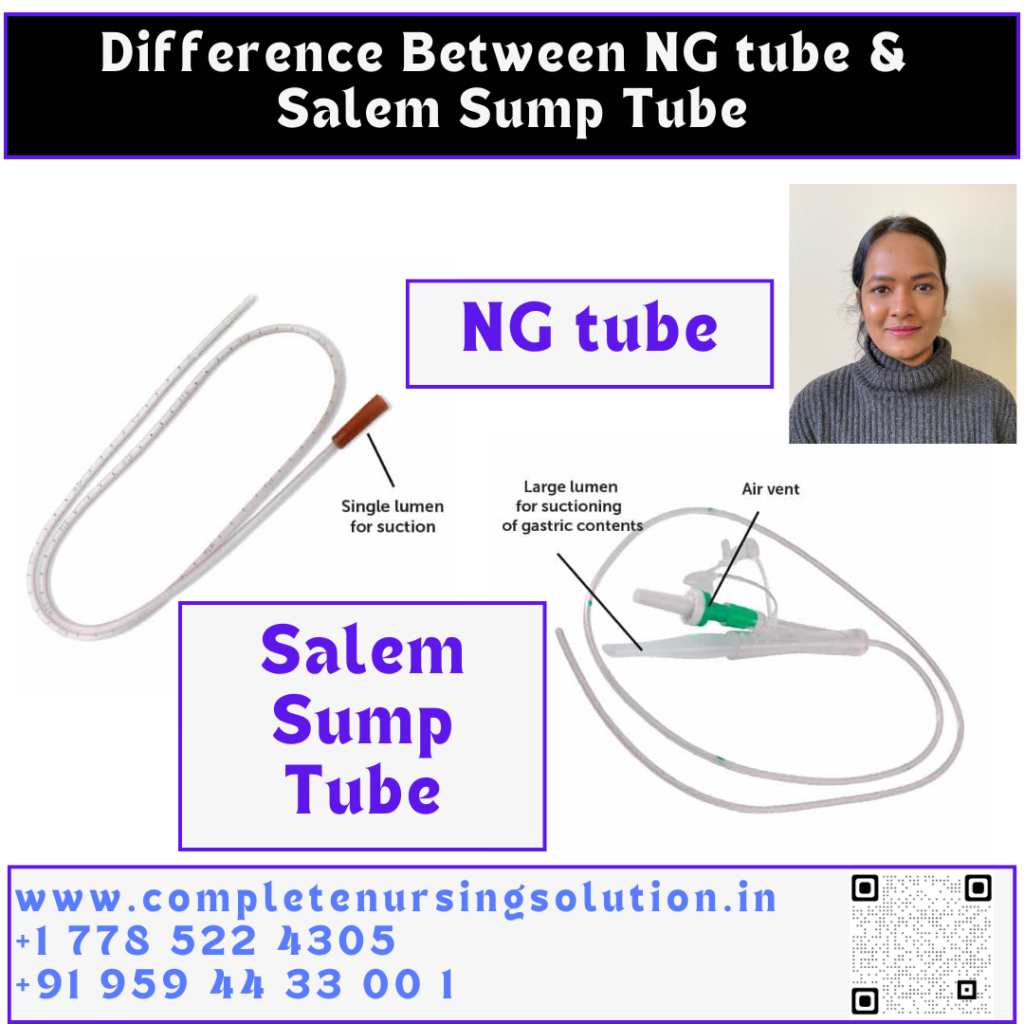
(Option 2) Hypoactive bowel sounds are typical after abdominal surgery as the bowel has been handled and manipulated. Clients often have a nasogastric tube for suction until bowel sounds return. The nurse should continue to monitor for bowel sounds and the presence of flatus.
(Option 4) A decreased or absent pulse, together with cool, pale, or mottled extremities, would be cause for concern. This client has warm extremities. Pulses should be compared with preoperative status and can be verified with a Doppler if needed.
Educational objective: The nurse should carefully monitor renal status in a client who has had abdominal aortic aneurysm repair. BUN, creatinine, and urine output should be assessed. Urine output of at least 30 mL/hr is expected.
Renal perfusion status is monitored closely in a client who has had abdominal aneurysm repair. Hypotension, dehydration, prolonged aortic clamping during surgery, blood loss, or embolization can lead to decreased renal perfusion and potential kidney injury. The nurse should routinely monitor the client's blood urea nitrogen (BUN) and creatinine levels as well as urine output. Urine output should be at least 30 mL/hr. This client should have an output of at least 120 mL of urine in a 4-hour period.
(Option 1) Diminished breath sounds in the lung bases are a common occurrence after surgery, especially in a client who has an abdominal incision that is painful with deep inspiration. The nurse should medicate the client for pain and encourage coughing, deep breathing, and use of an incentive spirometer.
(Option 2) Hypoactive bowel sounds are typical after abdominal surgery as the bowel has been handled and manipulated. Clients often have a nasogastric tube for suction until bowel sounds return. The nurse should continue to monitor for bowel sounds and the presence of flatus.
(Option 4) A decreased or absent pulse, together with cool, pale, or mottled extremities, would be cause for concern. This client has warm extremities. Pulses should be compared with preoperative status and can be verified with a Doppler if needed.
Educational objective: The nurse should carefully monitor renal status in a client who has had abdominal aortic aneurysm repair. BUN, creatinine, and urine output should be assessed. Urine output of at least 30 mL/hr is expected.
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
PP, WM, EVO, DG, AG, Microgaming, SA, VIVA Gaming,… 888slot com link các NPH Live Casino tiềm năng mang đến cho người chơi hàng loạt cơ hội nhận thưởng gấp 40 lần tiền cược ban đầu. Bạn có thể thử sức với các trò chơi mới lạ như: Fast Baccarat, Speed Roulette, Fan Tan,… TONY12-19
Darüber hinaus gibt es auch eine Promotion namens „Sonntagsfreispiele“, und Sie können 100 Freispiele erhalten.
Neue Nutzer erhalten direkt nach der registrierung casinoly ein Willkommenspaket, das risikofreies Erkunden ermöglicht.
Das Portfolio überzeugt mit einer Vielzahl von casino spielen führender Softwarehersteller wie NetEnt und Evolution Gaming.
Ob Sie Spannung bei Slots, Tischspielen oder Live-Dealer-Erlebnissen suchen – Casinoly
bietet eine rundum gelungene und lohnende Spielumgebung, die zu den besten der Branche zählt.
Meine Erkundung von Casinoly online casino ergab
eine ausgewogene Skala von Vorteilen und verbesserungswürdigen Bereichen. Sowohl die Desktop- als auch die mobilen Versionen von Casinoly online casino versprechen ein nahtloses Gameplay, das ein einheitliches Spielerlebnis
auf allen Geräten gewährleistet.
Die restlichen 180 Freispiele wurden für die nächsten 9 Tage
angekündigt –jeweils 20 Stück pro Tag.
Wir wählten 50 €, gaben die Transaktion über die App frei, und exakt 10 Sekunden später waren die
Mittel auf dem Spielerkontosichtbar. Doch bevor wir auf „Spielen“ klickten, ging es erstmal um die erste Einzahlung
und den Willkommensbonus. Besonders gut fanden wir, dass uns das Systemgleich nach dem ersten Login daran erinnerte, den Willkommensbonus zu
beanspruchen – kein Suchen, kein Rätselraten.
Das Casinoly Live Casino bietet eine breite Auswahl an Echtzeit-Spielen, darunter Live-Roulette, Blackjack, Baccarat
und spannende Game-Shows wie Dream Catcher. Zusätzlich gibt es
regelmäßige Aktionen wie Reload-Boni und Freispiele für Bestandskunden. Insgesamt bietet die Seite ein sicheres
und umfassendes Online-Casino-Erlebnis mit einer breiten Auswahl an Spielen, attraktiven Boni und exzellentem Kundenservice.
References:
https://online-spielhallen.de/robocat-casino-login-alles-was-sie-wissen-mussen/
This charming cafe offers more than just a culinary experience;
it is a journey through the annals of Georgian literature and culture.
Let’s look at the TOP 10 banks in Georgia, which are significant players in the market and have a high level
of customer trust. In conclusion, Tbilisi’s casino scene offers a diverse range of options for gambling enthusiasts.
Boasting an extensive game selection and regular live performances,
this establishment ensures a lively and entertaining experience.
With its high-end décor, top-notch facilities, and a variety of gaming options,
this casino is ideal for those seeking a touch of elegance.
With its friendly staff, excellent service, and diverse gaming options, this casino ensures a memorable visit.
Offers change frequently — check the Promotions page and your account notifications.
Check local laws in Australia and confirm you are of legal gambling age before registering with any casino.
Remember to read T&Cs, set responsible limits and
check your country laws to confirm you are legally eligible to play.
This block explains how audits work and how to verify fairness yourself.
References:
https://blackcoin.co/bsb007-casino-a-comprehensive-review/
Lower requirements make it easier to withdraw your winnings, while higher ones require more playtime.
For example, if you get a $100 bonus with a 30x wagering requirement,
you must wager $3,000 ($100 \\u00d7 30) before you can cash out.
While the site uses SSL encryption and reputable game providers, the licence does not offer
the same level of player protection as stricter regulators like
the MGA or UKGC.
The extensive game library, powered by Realtime Gaming (RTG), includes a variety of slot machines,
card games, and progressive jackpots. Ozwin Casino is
fortunate enough to provide gameplay on a range
of compatible devices. Finally, you can check out
Gambling Therapy for emotional support if you or your loved one is being impacted by problem gambling.System Requirements
Ozwin App is a popular online casino platform for players
who love exciting games and big bonuses. Established players earn regular casino promotions like Friday deposit bonuses, cashback bonuses, and weekly
giveaways. Loyal Ozwin players can claim exclusive casino bonuses and cashback
of up to 50%! The second deposit made by players at the
casino is also matched 200% to the value of $2000 and with this
match up bonus the player receives 50 free spins on the exciting Bubble Bubble 2 pokies game.
References:
https://blackcoin.co/harvest-buffet-the-star-sydney/
australian online casinos that accept paypal
References:
guateempleos.com
online casinos that accept paypal
References:
adpost4u.com
phtaya 63 https://www.phtaya-63.org
77jili https://www.77jilig.net
bk8casino https://www.bk8casinovs.com
Your article helped me a lot, is there any more related content? Thanks! https://www.binance.com/hu/register?ref=IQY5TET4